Endocannabinoid Deficiency: Symptoms, Causes, & Treatment
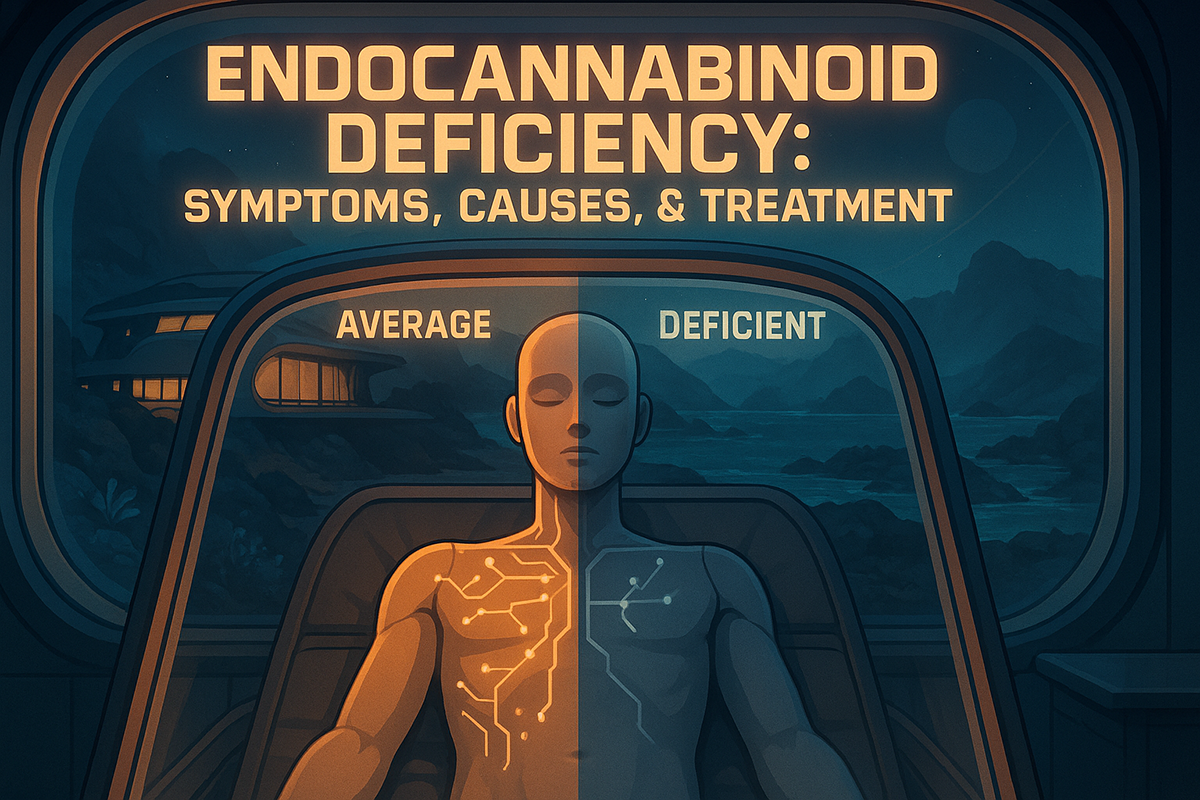
The endogenous cannabinoid system (ECS) helps keep your body in balance, so it only makes sense for everything to get thrown off when the ECS isn’t doing what it’s supposed to do.
The prevalence and clinical implications of clinical endocannabinoid deficiency (CECD or CED) are still being studied and remain only a theory so far. It’s based on the idea that maybe low levels of endocannabinoids are linked to pathophysiological syndromes that affect human health, similar to how neurotransmitter deficiencies are associated with many central nervous system disorders — from multiple sclerosis to psychiatric disorders.
Let’s look at what the studies show so far, the diseases implicated in endocannabinoid deficiencies, and how this affects medicine.
What is Clinical Endocannabinoid Deficiency (CED)?
Research and human studies say a dysfunctional endocannabinoid system can contribute to disease development or worsen its symptoms, and the consumption of phytocannabinoids helps bring balance back to the system, allowing it to function better. Can this concept explain the therapeutic benefits of cannabinoids in diseases?
To understand CED, you have to know the basics behind the endocannabinoid system (ECS) and its therapeutic potential.
The ECS regulates the following systems:
- Sleep and circadian rhythm
- Mood and stress
- Central nervous system (the brain and spinal cord)
- Peripheral nervous system
- Immune system
- Reproductive system and fertility
- Digestive system, gastrointestinal tract, intestinal motility, and appetite
- Hormones
- Arterial and respiratory system
- Skin health
- Pain, (acute and chronic pain as well as neuropathic pain)
- Appetite
- Inflammation, including neuroinflammation
- Motor control
- Temperature regulation
- Memory
- Pleasure/reward
- Cognitive function
Crucial? You bet.
Endocannabinoids anandamide (AEA, or the bliss molecule) and 2-arachidonoylglycerol (2-AG) act on the cannabinoid receptors CB1 and CB2, which are found in relative abundance in the brain regions and immune system. These receptors then send signals to specific parts of the human body, telling them to take an action of some sort. Certain enzymes, like the fatty acid amide hydrolase (FAAH), break down the endocannabinoids.
The theory is that a shortage of these endocannabinoids, such as in central anandamide deficiency, has clinical implications and causes health problems, as one would suspect. It doesn’t take a scientist to figure that out. These deficiencies could be caused by genetic or congenital defects, injury, or other diseases.
The problem is narrowing down what specific issues come up and what to do about them. Because the ECS does so much, it’s hard — almost impossible — to tweak one area without affecting the others.
Researchers have found many diseases that are possibly linked through an endocannabinoid deficiency, but migraines, irritable bowel syndrome, diarrhea, and fibromyalgia are the greatest evidence that it exists so far. These three, until now, appeared to have no cause and are, therefore, hard to diagnose. In fact, they tend to be written off as psychosomatic (“all in your head”). Medications and other treatments are hit-and-miss, usually resulting in a lifetime of care that really doesn’t do much.
We’ll look at the health problems that might be caused by low endocannabinoid levels, or possible symptoms, so to speak, of CED.
CED & Disease
If CED proves to be the underlying cause in even some of these functional disorders or health conditions, the door for new treatments will fly open. As we mentioned, it’s a matter of finding ways to fix one problem without causing more problems somewhere else. Still, researchers are finding ways to do this, which we’ll also discuss.
CED & Migraines, IBS, & Fibromyalgia
Migraines, IBS, and fibromyalgia might tend to go underdiagnosed and untreated, but why link them together beyond that? What do these three have in common that sets them apart?
They all share the following pathophysiological trends: (abnormal physical changes that happen because of a disease):
- Lack of characteristic tissue pathology or laboratory findings
- Diagnoses based on exclusion, after ruling out everything else
- Anxiety and depression are common
- Often labeled psychosomatic
- Comorbidity among the three diseases is high
- Patients with one are at high risk of developing one or both of the others
CED & Melancholic Depression
Melancholic depression, a subtype of major depression, can be more severe than general depression, though the symptoms are similar.
People with melancholic depression tend to move and speak slower, show little emotion, lose weight, sleep poorly but have increased wakefulness, feel extra sensitive to stress, and have trouble concentrating and remembering things. This usually accompanies strong feelings of guilt and thoughts of suicide.
Blocking the CB1 receptor causes a phenotypic state similar to melancholic depression — specifically, decreased appetite, increased anxiety and stress, wakefulness, and arousal — suggesting the ECS could play a role in the cause of it. There’s a possible further connection since some antidepressants increase endocannabinoid activity while chronic stress down-regulates it.
CED & Stress
More and more research is showing just how crucial of a role the ECS plays in regulating stress and stress induced anxiety by acting as a buffer to its effects. Changes in the system seem to affect aspects of the stress response.
In 2014, a study compared mice exposed to chronic stress with CB1 knock-out mice (the CB1 receptor was inactivated).
The mice under stress developed symptoms of depression, and the knock-out (KO) mice exhibited the same symptoms with or without added stress. KO mice had decreased 5-HTT levels under non-stressful situations, similar to the mice under stress. This study reveals a link between stress, depression, and the ECS.
CED & PTSD
In many studies, PTSD sufferers show reduced AEA and increased CB1 availability. There also seems to be a link between increased CB1 receptor availability in the amygdala, abnormal threat processing, and increased hyperarousal.
In fact, it’s almost a given that endocannabinoid levels in PTSD patients will be off. Previous attempts to study cannabinoid levels in blood samples of those with PTSD and those without it have been inconsistent. However, hair samples are proving to be a reliable way to assess these differences, and researchers are finding a significant difference in levels. Because of this, the ECS could be a target for treating PTSD.

CED & Huntington’s Disease
Reduced CB1 availability seems to be widespread in Huntington’s disease, which seems to repress its transcription. Huntington’s also causes a decrease in GABA, which might be linked to the ECS since it usually helps modulate GABA.
Other Possible Problems From CED
While finding new treatments for any or all of the above would be fantastic, there are other areas the CED might impact, especially when it comes to other treatment resistant conditions. The following all remain treatment-resistant and show unexplained symptoms.
- Cystic fibrosis
- Causalgia
- Phantom limb pain
- Brachial plexopathy
- Neonatal failure to thrive
- Infantile colic
- Glaucoma
- Dysmenorrhea
- Hyperemesis gravidarum
- Bipolar disease
- Repetitive miscarriage
Is There a Solution to CED?
While finding the right balance could be difficult, research shows that it might not take much of a bump to get the ECS working right. Instead of a complete overhaul, a small nudge could provide amazing results.
There are, potentially, a number of ways to increase endocannabinoid levels — specifically AEA — though more research is needed before we come to any conclusions.
- MGL and FAAH-inhibitors
- CB1 or CB2 agonists or partial agonists
- Inhibiting endocannabinoid transport
- Modulating ECS function through allosteric sites
- Glucocorticoid hormones
- Lifestyle changes, such as low-impact aerobic exercise and diet

FAAH (fatty acid amide hydrolase) is an enzyme that breaks down AEA, and MGL (monoacylglycerol lipase) breaks down 2-AG. Slow down this process, and you have more available endocannabinoids.
Phytocannabinoid Wannabes
Cannabinoids aren’t quite exclusive to cannabis, though it sure seems so. It’s certainly the best place to find them. Most plants don’t contain arachidonic acid, an essential ingredient in binding to receptors. However, some plant compounds like to pretend they’re cannabinoids. Here are some examples of plant ‘ingredients’ that exhibit cannabinoid-like behavior.
1. N-alkylamides (Alkamides)
Echinacea contains certain alkamides that can interact with CB2 receptors, slow down AEA reuptake, and show similar effects as AEA.
2. Falcarinol
The common plant Daucus carota (carrots) contains falcarinol, which binds to both receptors. This goes through an alkylation reaction with CB1, resulting in a strong inverse agonistic effect.
3. Salvinorin A
The research goes back and forth on salvinorin A, the main active molecule in Salvia divinorum, a dissociative hallucinogenic plant. In some studies, it did not show binding to CB1 activity, but whole leaves from the plant did. Other studies showed it interacted with CB1 and k-opioid receptor dimers, suggesting a possible connection between the two.
4. Yangonin
Yangonin is a major component of kavalactone, the active compound in Piper methysticum, or kava. We’ve known it has GABAB receptor activity, but current research shows it binds to CB1 receptors — it’s unclear whether the activity is antagonistic or agonistic.
5. Beta-Caryophyllene
Beta-caryophyllene is a terpene common in cannabis, but it’s plenty abundant elsewhere, too — hops, black pepper, and cloves, to name a few. It’s possibly the only terpene that interacts with CB receptors. In this case, it’s a full agonist of CB2.
FAQs on the Endocannabinoid System
The ECS is a powerful biological system that helps regulate many bodily functions. The section below discusses some of the commonly asked questions about the ECS.
1. What is the Difference Between Endocannabinoids and Cannabinoids?
Endocannabinoids (endogenous cannabinoids) are compounds produced by our cells in response to stimulus. On the other hand, cannabinoids (phytocannabinoids) are compounds produced by the cannabis plant, and these include THC, CBD, CBC, CBG, and CBN, among others.
2. What Part of the Body Has the Most Cannabinoid Receptors?
The brain has the most cannabinoid receptors, especially type 1 receptors. The immune system, on the other hand, has the most type 2 cannabinoid receptors.
3. What Triggers the Release of Endocannabinoids?
Various stimuli can trigger the release of endocannabinoids. These include but are not limited to pain, inflammation, fear, anxiety, and hunger. Good stimuli also activate the cells to release endocannabinoids, such as exercises, laughter, massage, and intimacy or sexual activities.
4. How Do I Know If I Have Endocannabinoid Deficiency?
There’s no specific or standardized test that checks for endocannabinoid deficiency. However, the endocannabinoid levels can be measured in laboratory settings using techniques such as mass spectrometry and immunoassay.
5. What are the Symptoms of Low Cannabinoids?
Because the ECS regulates many bodily functions, the symptoms of low endocannabinoids vary, from headaches and nausea to restlessness and mood changes. Weight gain and weight loss may also be symptoms of endocannabinoid deficiency.
6. What Destroys the Endocannabinoid System?
Chronic medical conditions, may it be physical or mental health issues, put unnecessary strain on the endocannabinoid system and affect its health, resulting in deficiencies and a dysfunctional ECS.
7. What are the Disorders of the Endocannabinoid System?
Dysfunctional ECS has been implicated in many diseases and disorders — from chronic treatment-resistant pain and low-grade inflammation to Huntington’s and Alzheimer’s diseases.
8. How to Fix the Endocannabinoid System?
Just like maintaining a healthy body, you can “fix” or maintain ECS health by a good diet, regular exercise, restful sleep, and meditation.
9. How to Make Your Body Produce More Endocannabinoids?
You can produce more endocannabinoids the natural way through physical activities like exercise. Managing stress, getting enough rest and sleep, and avoiding bad habits like smoking and drinking can also increase endocannabinoid levels.
10. What Foods Affect the Endocannabinoid System?
Good foods rich in essential fatty acids like sardines, eggs, flax seeds, walnuts, or olive oil help improve ECS health. On the other hand, foods high in sugar, fat, salt, or bad carbohydrates damage the ECS
References Used
- Russo, E. B. (2016). Clinical endocannabinoid deficiency reconsidered: current research supports the theory in migraine, fibromyalgia, irritable bowel, and other treatment-resistant syndromes. Cannabis and cannabinoid research, 1(1), 154-165 [1].
- Hill, M. N., & Gorzalka, B. B. (2005). Is there a role for the endocannabinoid system in the etiology and treatment of melancholic depression? Behavioural pharmacology, 16(5-6), 333-352.
- Morena, M., Patel, S., Bains, J. S., & Hill, M. N. (2016). Neurobiological interactions between stress and the endocannabinoid system. Neuropsychopharmacology, 41(1), 80-102 [3].
- Burokas, A., Martín‐García, E., Gutiérrez‐Cuesta, J., Rojas, S., Herance, J. R., Gispert, J. D., … & Maldonado, R. (2014). Relationships between serotonergic and cannabinoid system in depressive‐like behavior: a PET study with [11C]‐DASB. Journal of Neurochemistry, 130(1), 126-135 [4].
- Neumeister, A., Seidel, J., Ragen, B. J., & Pietrzak, R. H. (2015). Translational evidence for a role of endocannabinoids in the etiology and treatment of posttraumatic stress disorder. Psychoneuroendocrinology, 51, 577-584.
- Wilker, S., Pfeiffer, A., Elbert, T., Ovuga, E., Karabatsiakis, A., Krumbholz, A., … & Kolassa, I. T. (2016). Endocannabinoid concentrations in hair are associated with PTSD symptom severity. Psychoneuroendocrinology, 67, 198-206 [6].
- Van Laere, K., Casteels, C., Dhollander, I., Goffin, K., Grachev, I., Bormans, G., & Vandenberghe, W. (2010). Widespread decrease of type 1 cannabinoid receptor availability in Huntington disease in vivo. Journal of Nuclear Medicine, 51(9), 1413-1417.
- Allen, K. L., Waldvogel, H. J., Glass, M., & Faull, R. L. M. (2009). Cannabinoid (CB1), GABAA and GABAB receptor subunit changes in the globus pallidus in Huntington’s disease. Journal of chemical neuroanatomy, 37(4), 266-281 [8].
- Hill, M. N., Campolongo, P., Yehuda, R., & Patel, S. (2018). Integrating endocannabinoid signaling and cannabinoids into the biology and treatment of posttraumatic stress disorder. Neuropsychopharmacology, 43(1), 80-102.
- Vemuri, V. K., & Makriyannis, A. (2015). Medicinal chemistry of cannabinoids. Clinical Pharmacology & Therapeutics, 97(6), 553-558.
- Russo, E. B. (2016). Beyond cannabis: Plants and the endocannabinoid system. Trends in pharmacological sciences, 37(7), 594-605.
- Capasso, R., Borrelli, F., Cascio, M. G., Aviello, G., Huben, K., Zjawiony, J. K., … & Izzo, A. A. (2008). Inhibitory effect of salvinorin A, from Salvia divinorum, on ileitis‐induced hypermotility: cross‐talk between κ‐opioid and cannabinoid CB1 receptors. British journal of pharmacology, 155(5), 681-689.